The Impact of COVID-19: Primary Procedures Performed During & After Elective Surgery Mandates
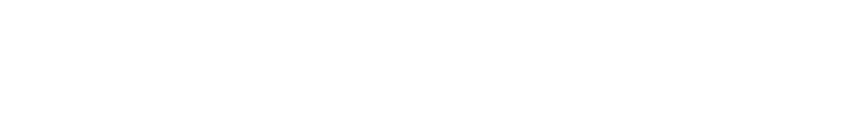
As the COVID-19 virus reached its initial peak confirmed case count in April, several states mandated the reduction of elective surgeries not deemed medical necessities. According to data organized on the COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University the United States collectively witnessed new Daily Cases of COVID-19 in the range of 30-40k.
The US crossed 70k new Daily Cases for the first time on July 16th, 2020. In the event of a second mandate postponing non-essential surgeries, what can we learn from the first? What does the data from outpatient ambulatory surgery centers (ASCs) tell us about the surgical procedures most likely to be performed and those most at-risk of being delayed?
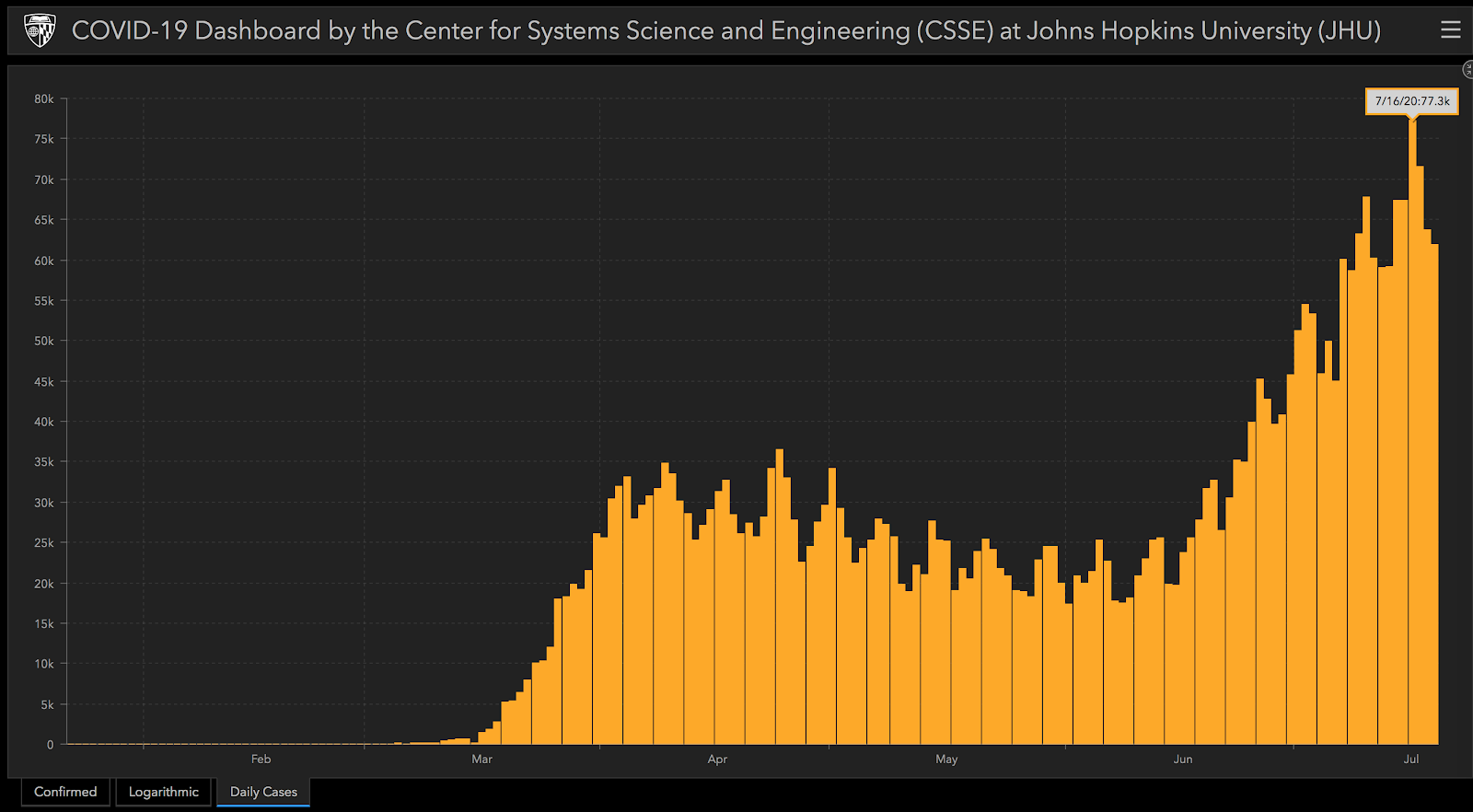
Primary Procedure Performed During Elective Surgery Suspension
Below is an analysis of performed surgeries from three ASCs in a shared state that mandated the postponement of non-essential elective surgery.
Fractures and Demobilizing Injuries
The most notable insight derived from an analysis of the procedures performed during the elective surgery shutdown is the 883% increase in prevalence of procedures treating fractures or other trauma-related, demobilizing injuries to tendons. This result supports the state mandate to postpone elective surgeries, which would not include demobilization and fractures that are medically necessary and ongoing.
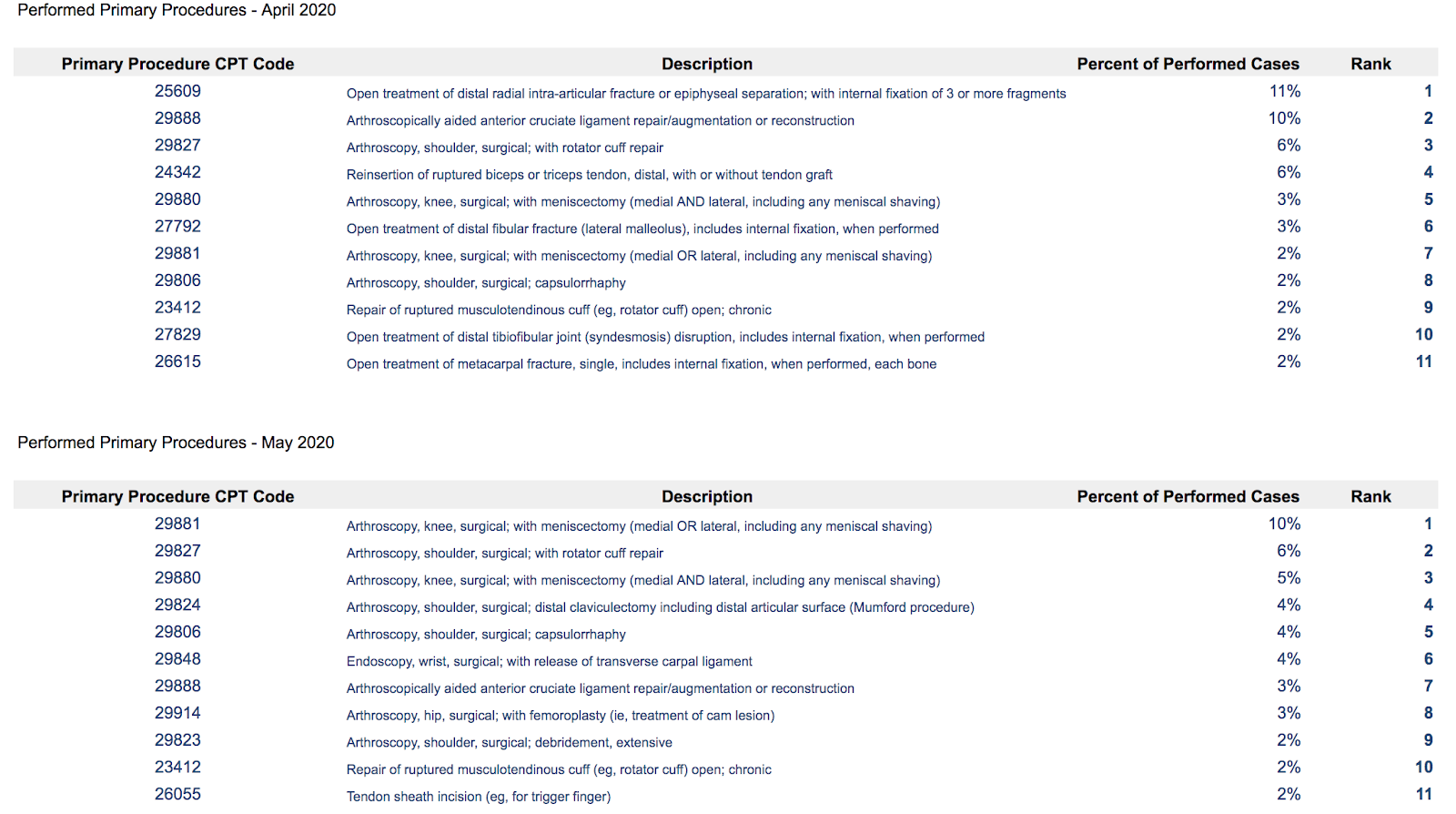
What is more, should there be a second mandate to postpone additional surgeries in July, August, or September (as already witnessed in Texas and Florida), we can expect more fractures and trauma-related procedures to be performed in the outpatient setting due to a higher incidence rate of causative injuries during summer months.
According to a five-year study published in The Orthopedic Journal at Harvard Medical School:
“Higher temperatures and longer days were predictive of higher volume of total injuries and open fractures. There is seasonal variability in adult orthopaedic trauma with higher volume and open fractures occurring in the summer months.”
http://www.orthojournalhms.org/19/article46_51.html
Conclusion
2020 is a year unlike any we’ve experienced in the vast majority of our lifetimes. It’s worth noting that the seasonality of injuries this year may be wildly different from past years, given social distancing measures and the cancellation or postponement of sport seasons.
Yet even so, we can expect the outpatient setting to shift its focus to the treatment of fractures and other trauma-related injuries in the event of additional mandated suspensions of elective surgeries. The fear of visiting hospitals may also contribute significantly to this procedure growth - in the short term and long term. When COVID-19 tore through New York City in April of this year, Emergency Room visits were down nearly 50%. With respect to battling the pandemic, this is not an unwelcome outcome as the reduction in ER visits increases the available beds to treat patients suffering from COVID-19.
Ambulatory Surgery Centers (ASCs) are having an unsolicited moment in the spotlight, proving that smaller facilities that are geographically distributed can safely serve as a vital piece of the healthcare infrastructure - especially in critical moments of procedure outgassing from their larger, more centralized hospital counterparts.
Questions, comments, additions? Let us know.
Learn more about Relatable Healthare and how we can help you better manage the business of surgery.